By Lucy Gleysteen
From PHN Issue 44, Fall 2020
As of October 2020, at least 1 million people worldwide and 200,000 people in the United States have died of COVID-19. Experts say that the true number of deaths is higher than what has been reported. In the United States, the number of deaths would have been lower had there been wide-scale testing, contact tracing, mask wearing mandates, accessible personal protective equipment for essential workers, and large-scale quarantining. COVID-19 still persists, and the number of deaths continues to rise. Case counts on the outside are trending upwards, reaching peak levels in some places.
Over the course of the spring and summer, COVID-19 cases have soared in prisons across the United States. In prisons and jails, infectious diseases spread quickly because the conditions of incarceration force people into crowded living situations without access to proper safety and prevention measures.
How is COVID-19 spread?
The virus that causes COVID-19 spreads through person-to-person contact, most often through respiratory droplets. Respiratory droplets are small particles that come from a person’s mouth or nose. Droplet transmission occurs when a person who has COVID-19 coughs, sneezes, or talks near someone else and they inhale the particles. The Center for Disease Control provides guidance that people should stay at least six feet apart to prevent the transmission of COVID-19. However, it is still possible for COVID-19 to be transmitted from farther away if someone who has COVID-19 is in an enclosed space with few windows and poor ventilation. This is called airborne transmission. In enclosed spaces with other people, there is the possibility of contracting COVID-19 because those environments contribute to the buildup of virus-carrying particles in the air. This possibility is also higher if people are doing activities that can release more virus-carrying particles into the air, like shouting, singing, or exercising. It is still possible to contract COVID-19 from touching objects and then touching your eyes, nose, or eating. It is important to wipe down surfaces and frequently wash your hands to reduce risk. Strategies to avoid COVID-19 are often harder in prison than for people on the outside. These strategies include staying at least 6 feet away from other people, wearing a mask that covers the nose and mouth, washing hands frequently, and to the extent that it’s possible, avoiding crowded spaces.
What’s it like to get COVID-19?
Most people who contract COVID-19 experience mild to moderate symptoms and recover without medical intervention. However, serious illness can develop. People over the age of 65 or who have pre-existing conditions such as cancer, being immunocompromised, chronic kidney disease, heart conditions, sickle cell disease, and diabetes are at increased risk for complications from COVID-19. The most common symptoms of COVID-19 include a fever, dry cough, tiredness, and shortness of breath. Additional symptoms include congestion, sore throat, headache, diarrhea, muscle and body aches, and/or new loss of taste or smell.
When to seek immediate medical attention
If someone is having trouble breathing, chest pain or pressure, confusion, an inability to wake or stay awake, or looks blue in the face or lips, seek immediate medical attention.
Long-term impacts of COVID-19
Many of the long-term effects of COVID-19 remain unknown because it is a new illness. The long-term impact of COVID-19 varies depending on the person. While some people are able to clear the virus and recover after a few weeks, others experience COVID-19 symptoms for months. The virus can damage the lungs, heart, and brain, which can lead to serious long-term health issues.
For some people, COVID-19 has affected their hearts by causing inflammation and damage to the heart muscle. Heart damage is a part of what can cause COVID-19 to be severe and deadly, for people of any age. The impact of COVID-19 on the heart may be the cause of some of the long-term symptoms people have reported after COVID-19. This includes shortness of breath, chest pains, and heart palpitations. Another serious side effect of COVID-19 is the possibility of a stroke. COVID-19 can cause blood clots that travel throughout the body and lead to stroke. This can happen to people of all ages. Some people experience cognitive difficulties during and after having COVID-19. This includes memory loss, confusion, dizziness, difficulty focusing, and brain fog.
Is there a vaccine yet?
Researchers around the world are working to find a vaccine for COVID-19. Vaccines usually take years of research and testing before they become available to the public. This process is being accelerated for the COVID-19 vaccine due to the wide-scale health and economic devastation the pandemic has caused. At the moment, there are many different vaccines that are being tested for COVID-19. Some of these options have been promising, but more data is still needed. When a vaccine is approved, there is no way of knowing how long it will take to get everyone vaccinated. Having an effective vaccine would be a significant step in ending the pandemic. However, it will only work if researchers are certain that the vaccines are effective and safe.
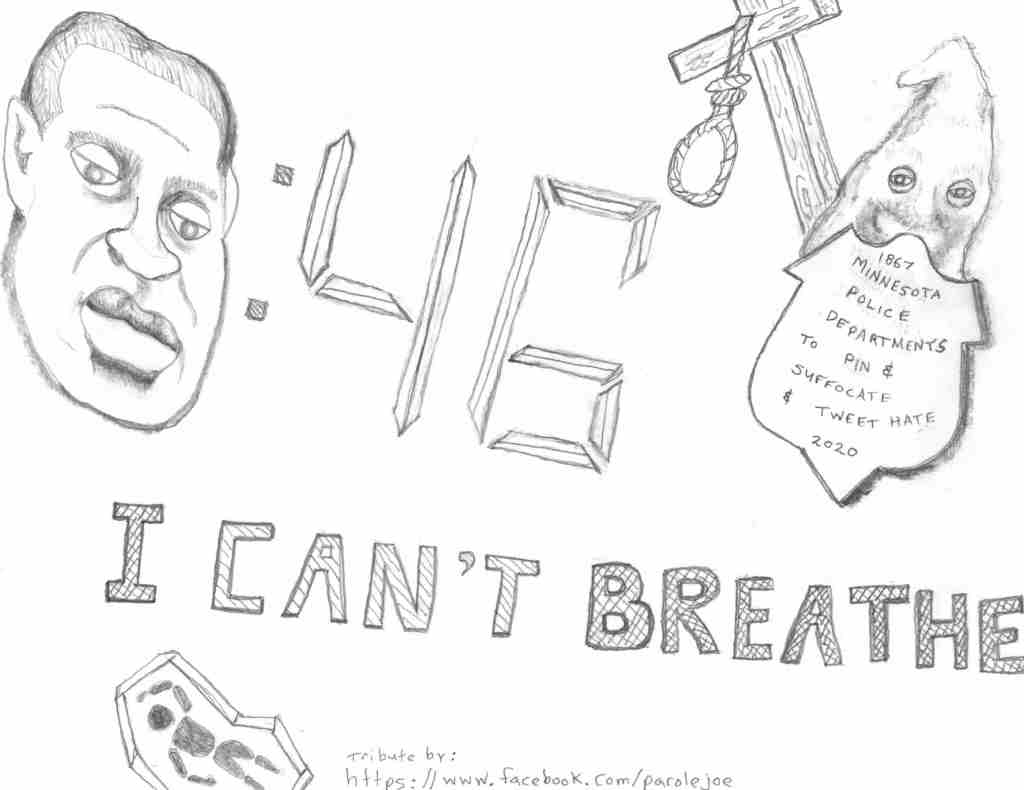
Who is most impacted by COVID-19?
While COVID-19 impacts everyone, those who experience systemic oppression are most vulnerable to contracting the virus and experiencing symptoms. This includes people in prison, people living in poverty, the elderly, essential workers, people with chronic illnesses and disabilities, undocumented people, people of color, and many more not mentioned. People who cannot work from home are vulnerable because they face the possibility of a COVID-19 exposure in order to earn a living. Factors that contribute to increased risk, especially for Black and indigenous people, include discrimination in healthcare systems, housing, education, and criminal justice. Not only does this lead to toxic stress, which can harm the immune system, but it also impacts who receives healthcare and the quality of healthcare they receive. A person’s geographic location and their local government can have an impact on risk if they live in a part of the country where COVID-19 is not taken seriously.